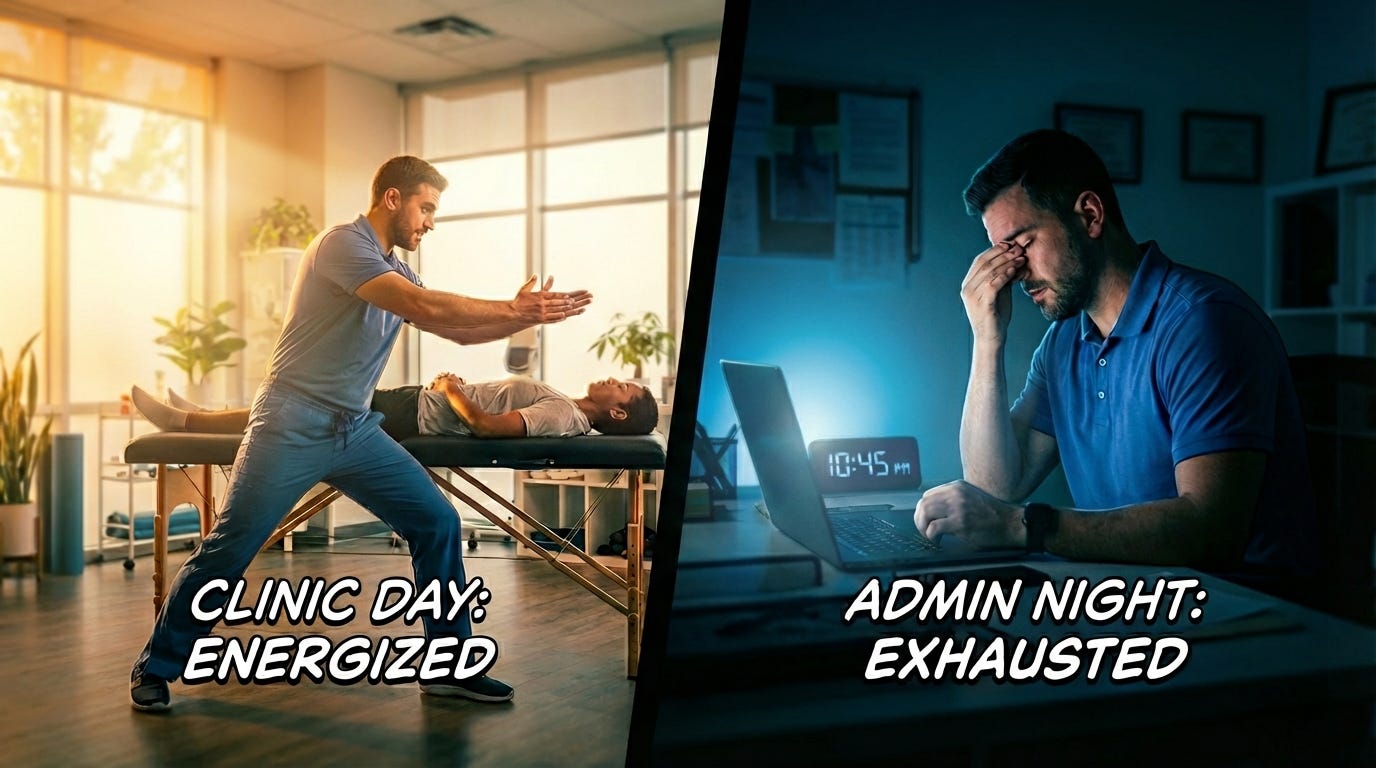
The 9pm Confession: What Your Family Already Knows About Your Documentation Burden
It’s 9:03 PM. Your kids went to bed 45 minutes ago. You gave them rushed hugs, promised you’d read longer tomorrow night, and listened to them complain that you’re always on the computer.
They’re right.
You’re sitting at the kitchecn table with your laptop. The blue glow is familiar. The routine is automatic. Open your EMR. Log in. Start working through the seven notes you didn’t finish during clinic hours.
Mrs. Johnson’s shoulder follow-up. The new low back eval. The Medicare patient who needs updated goals for the continuing treatment form.
You told yourself you’d be done by 9:30. You said that last Tuesday too.
This is Pajama Time. And if you’re reading this, you know exactly what I’m talking about.
The Statistic Your Spouse Could Have Told You
Here’s a number that won’t surprise you: 20.9% of healthcare professionals spend more than 8 hours per week on documentation outside normal work hours.
That’s the polite version.
The real version? Family medicine physicians average 86 minutes of “pajama time” with their EHR every single night. Not occasionally. Not when it’s busy. Every. Single. Night.
And physical therapists? 57% cite excessive documentation as the leading cause of burnout. For every hour you spend working on patient documentation at home, your odds of burnout increase by 2%.
The math is brutal. If you’re spending 1-2 hours at home every night finishing notes, you’re systematically increasing your burnout risk by 2-4% per night. Five nights a week. Fifty weeks a year.
Your family doesn’t need a research study to tell them you’re exhausted. They already know.
The Invisible Second Shift
Here’s what the industry won’t tell you: After-hours documentation is unpaid labor disguised as “catching up.”
You clock out at 5:30 PM. Your workday is officially over. But you’re not done working.
Between 5:30 PM and 7:00 AM on weekdays (plus weekends), you’re still in the EMR. Still documenting. Still billing. Still responding to inbox messages and prior auth requests and compliance alerts.
49% of a PT provider’s workday is consumed by administrative tasks and documentation. For every hour you spend treating patients, you spend nearly an equal amount documenting that care.
But here’s the problem: That second hour isn’t happening during clinic time. It’s happening after your kids go to bed.
This is the invisible second shift. And it’s destroying your work-life balance one SOAP note at a time.
The Quality Problem Nobody Talks About
Here’s the part that should terrify you: **9 PM documentation is worse than 3 PM documentation.**
Your clinical reasoning at 9 PM, after a full day of patient care, is not as sharp as it was at 9 AM. Your attention to detail is compromised. Your ability to recall specific patient interactions is fading.
So you’re not just working longer hours. You’re producing lower-quality notes during those hours.
Research on physician decision-making shows that cognitive fatigue leads to:
- Increased diagnostic errors
- Reduced attention to detail
- Higher likelihood of missing important clinical information
- More copy-paste errors (using old notes as templates without proper updates)
You know this is true because you’ve caught yourself doing it. You’ve copy-pasted last week’s objective findings and almost forgot to update them. You’ve documented “patient tolerated treatment well” because you can’t remember the specific details anymore.
And then you lie awake at night wondering if you documented enough to justify the billing codes. Or if you documented too much and created compliance risk.
This isn’t a personal failing. It’s a system design failure.
Why “Just Get Better at Time Management” Is Gaslighting
At some point, someone has probably told you that the solution to after-hours documentation is better time management.
Document in the room. Use templates more efficiently. Block out admin time during the day. Stop being a perfectionist.
This advice is well-intentioned. It’s also gaslighting.
Because the problem is not your time management skills. The problem is the system you’re working in.
Your EMR requires manual data entry for every single patient interaction. It doesn’t matter how fast you type or how good your templates are. You’re still the human typing into the machine.
Your billing compliance requirements demand detailed documentation. Medicare wants specificity. Insurance companies want justification. If you don’t document it, it didn’t happen. If you don’t document it correctly, you get audited.
Your clinic’s patient volume doesn’t include admin time. You’re scheduled for 12-15 patients per day with 45-minute to 60-minute appointment slots. That schedule assumes you’ll document outside of patient care time. Which means you’ll document after hours.
This isn’t a time management failure. This is architectural design.
Your EMR was designed to store information, not to reduce your workload. Your documentation requirements were designed to protect payers, not to respect your time. Your clinic schedule was designed to maximize revenue, not to include realistic admin time.
Telling burned-out PTs to “just manage your time better” is like telling someone to bail water faster while ignoring the hole in the boat.
What Your Family Sees (That You’ve Stopped Noticing)
Your spouse sees you at the kitchen table every night. Laptop open. Shoulders tense. Barely present.
Your kids stopped asking you to play after dinner because the answer is always “Maybe later” or “I need to finish my notes first.”
Your friends stopped inviting you to weeknight plans because you always say you’re too busy.
You’ve stopped booking evening plans because you know you’ll be working.
This is what “Pajama Time” actually means: The systematic erosion of your personal life in service of administrative tasks that should have been automated a decade ago.
Your family has adjusted to your absence. That should terrify you.
Because they shouldn’t have to adjust. You shouldn’t have to choose between documenting patient care and being present for your own life.
The System Is the Problem, Not You
Let me be absolutely clear: If you’re working until 9 PM every night to finish documentation, that is not a reflection of your competence, your speed, or your time management skills.
It’s a reflection of a broken system that:
1. Treats clinicians as data entry operators instead of healthcare professionals
2. Designs billing compliance rules that require excessive documentation to protect payers, not patients
3. Schedules patient volumes without accounting for realistic admin time
4. Normalizes unpaid after-hours labor as “part of the job”
5. Sells EMRs as solutions when they’re actually storage systems that require constant human input
The system is broken. You are not.
You are a skilled clinician who deserves to go home at 5:30 PM and actually be done with work.
You deserve to have dinner with your family without thinking about whether you documented the correct MMT grades.
You deserve to sleep without worrying about billing compliance.
You deserve to work one job, not two.
The Way Out (Yes, There Is One)
This article is part of Week 1 of Physiogentic, where I’m documenting the crisis. Next week, I’ll show you the solutions.
But here’s the preview: Real-time documentation and Agentic AI are the only paths out of this trap.
Not faster templates. Not better time management. Not “just document in the room” advice that ignores the reality of patient care.
Real-time ambient documentation that captures your clinical session without requiring you to type.
Agentic AI that drafts your note, generates your billing codes, and checks for compliance issues while you’re walking to your next patient.
Human-in-the-loop systems where you review and approve, not type and create.
This technology exists. Right now. It’s not theoretical. Clinics are already using it.
Mass General Brigham research shows that ambient documentation combined with virtual scribes reduced after-hours work by 42% and documentation delays by 66%.
That’s not a 5% improvement. That’s life-changing.
Imagine finishing your last patient at 5:15 PM, reviewing their auto-generated note on your phone while walking to your car, approving it with one tap, and being done.
Actually done.
Home by 5:45 PM. Present for dinner. No laptop at the kitchen table. No guilty glances at your kids while you’re “just finishing one more note.”
That’s not a fantasy. That’s the Agentic Era.
One More Thing Before You Close This Tab
This isn’t a productivity problem. It’s a design flaw.
You shouldn’t have to choose between your patients and your life.
That’s why we are building something different.
Next Week: Workflows Every PT Clinic Should Automate First (And Exactly How to Do It)
Sources
- Doctors work fewer hours, but the EHR still follows them home | American Medical Association
- Burnout on the way down, but “pajama time” stands still | American Medical Association
- Family doctors spend 86 minutes of “pajama time” with EHRs nightly | American Medical Association
- Electronic documentation burden among outpatient rehabilitation therapists | PMC
- Physical Therapist Burnout: What Role Does Documentation Play? | Net Health
- Role conflicts of physicians and their family members | PMC
- Who Is Caring for Health Care Workers’ Families Amid COVID-19? | PMC
- Hybrid Ambient Documentation Decreases After-Hours Work | Mass General Brigham